Deep Anterior Lamellar Keratoplasty (DALK) is indicated to correct conditions which result in corneal thinning, distortion or scarring such as advanced Keratoconus, LASIK or Radial Keratotomy induced corneal thinning, corneal dystrophy, infection or trauma .
DALK is an elegant partial thickness graft that unlike full-thickness corneal transplatation (PK), preserves the TWO inner most layers of the cornea: Descemet’s membrane and the endothelium, while removing and replacing only the diseased, weakened or scarred anterior layers with donor tissue. If the endothelial layer is normal, then it is worth preserving!
| [kml_flashembed movie=”https://www.icanseeclearly.com/wp-content/uploads/2011/05/fig8a.swf” height=”260″ width=”450″ /] |
| DALK: Cross section of cornea showing partial thickness cornea graft. Note: Descemet’s membrane and endothelial cell layer is retained and NOT replaced. |
Retention of this important layer not only may make a DALK graft last a lifetime and avoid rejection, but also makes the creation of larger diameter grafts possible. Since 2007, Dr. Erdey has refined techniques which permit the creation of larger diameter DALK grafts which tend to have less astigmatism, optical aberration and are associated with more rapid optical rehabilitation than smaller diameter grafts.
Read: Large-diameter DALK technique minimizes post-operative astigmatism – Richard A. Erdey, M.D.
Although DALK represents over 50% of the cornea grafts performed by Dr. Erdey and his team, very few cornea specialists offer this extremely delicate, time intensive and poorly reimbursed procedure despite it’s many benefits. In 2012, only 751 DALK’s were performed in the USA. About 20,000 eyes had full-thickness traditional corneal transplants when the vast majority may have been suitable DALK candidates. Dr Erdey frequently speaks and teaches at local and national conferences to his colleagues in an effort to reduce the barriers to surgeon acceptance. He passionately believes broader surgeon acceptance and conversion to DALK will eventually occur.
See Dr. Erdey’s case studies below:
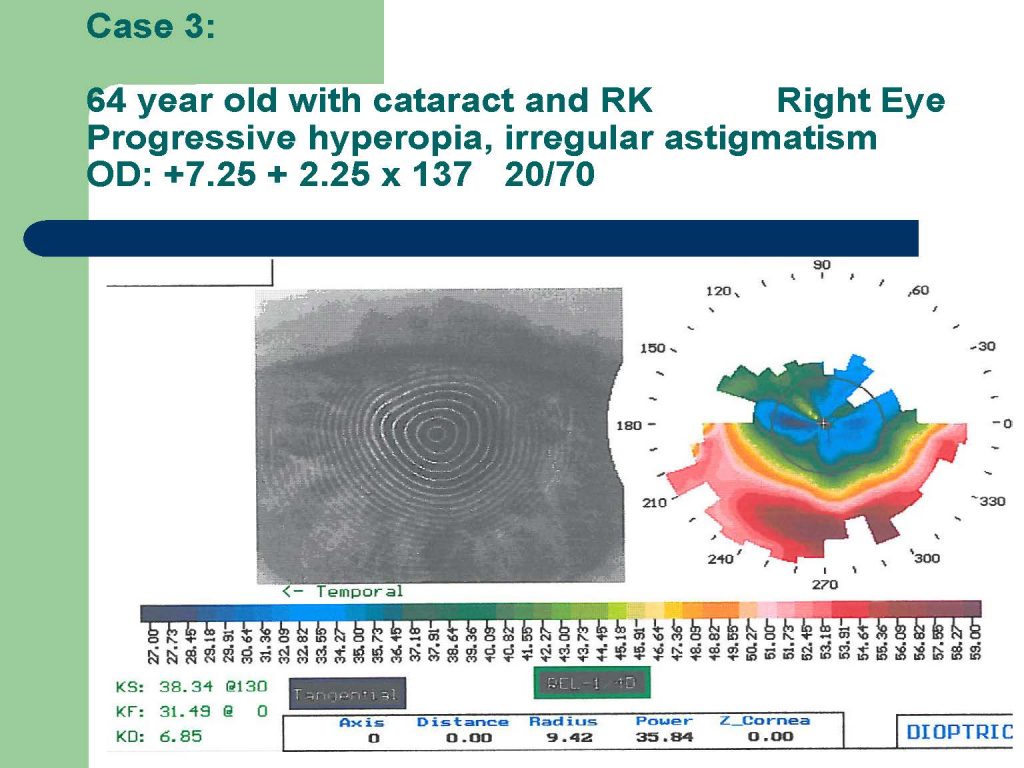
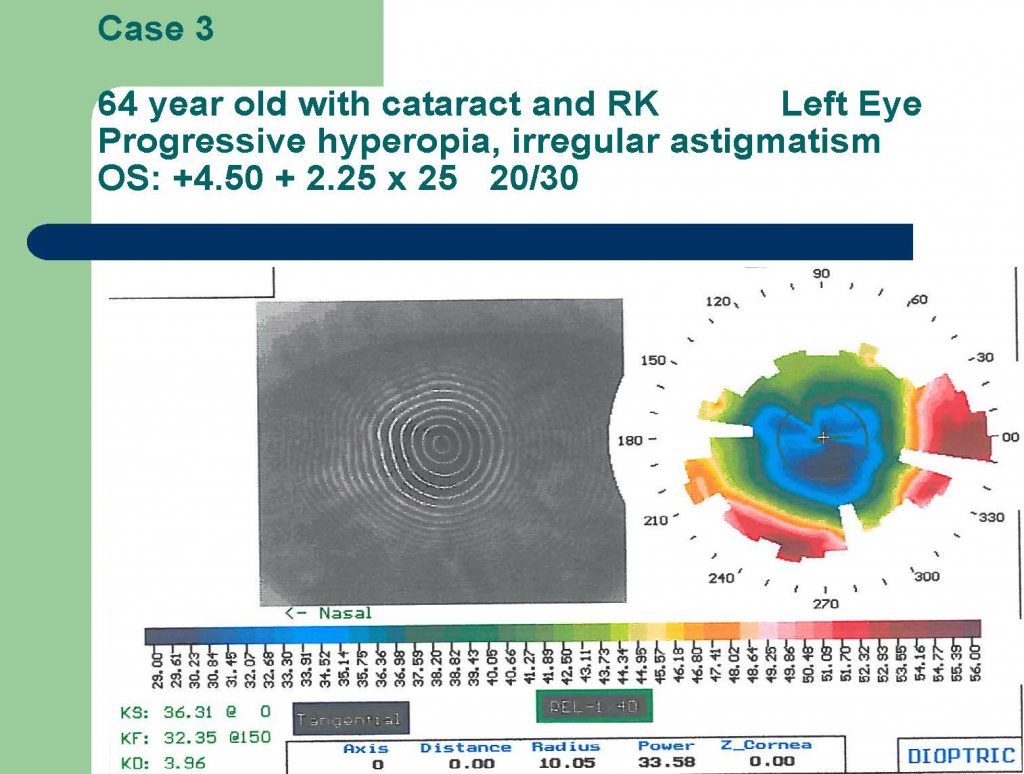
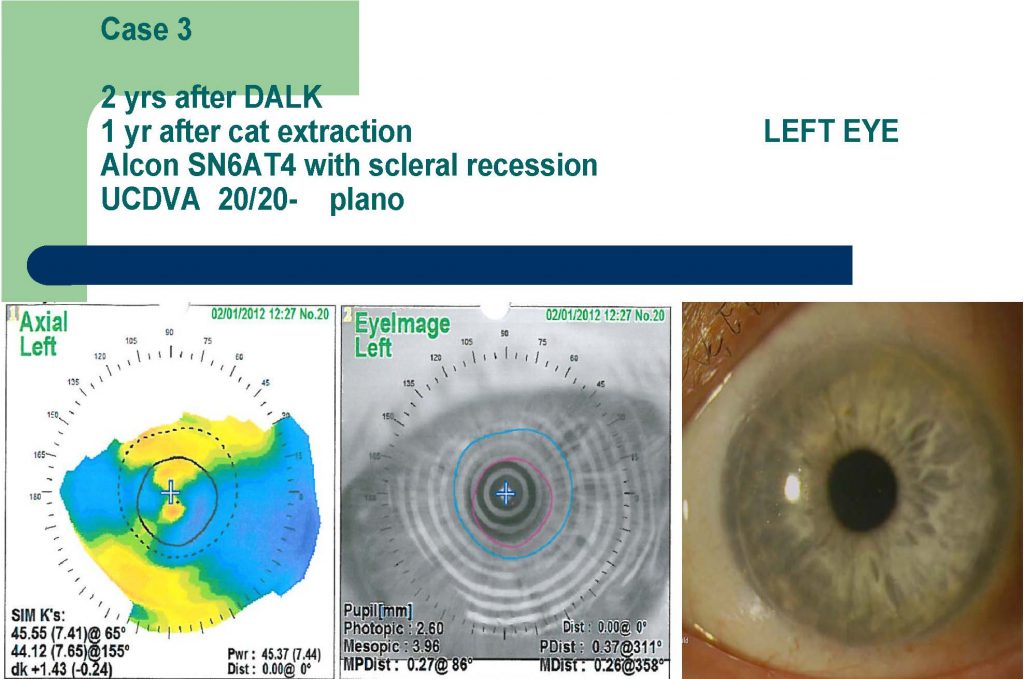
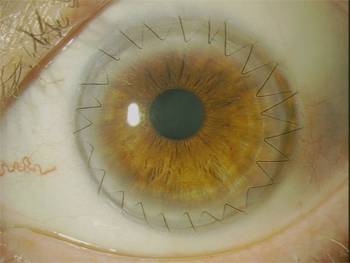 |
Case 1: Cornea after DALK: donor graft applied to retained recipient descemet’s membrane. Cornea transparency is restored. Sutures generally removed after 6 mos. |
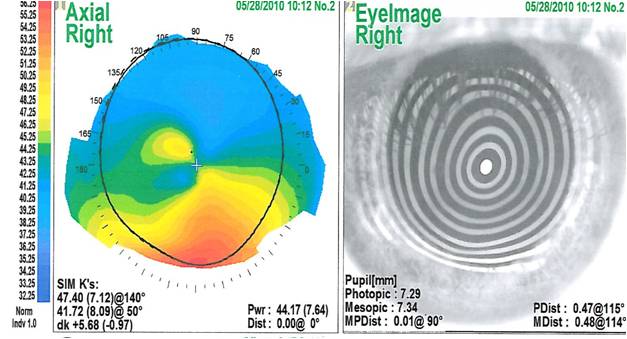 |
| Case 2: LASIK Induced Ectasia/Keratoconus: Rx: -7.0 + 7.0 x 135 x 20/60 Note distorsion of corneal mires on the image (right) |
 |
| Case 2: Cornea after DALK: sutures removed. Note: minimal astigmatism as demonstrated by corneal topography (left) and refraction: +1.25 +1.5 x 175 20/20- , resolution of corneal distortion (middle), large diameter corneal graft (right). The patient’s own Descemet’s membrane and endothelial cell layers are retained! |
The most suitable candidates for this procedure generally include those with healthy cornea endothelium, no descemet’s membrane scarring and who have:
» Keratoconus, or LASIK-induced corneal ectasia (thinning) who are gas permeable hard contact lens intolerant and are poor candidates for INTACS
» cornea scarring restricted to the bowman’s membrane or stroma
» cornea surface warpage (irregular astigmatism) who are intolerant of hard contact lenses
» complications from Radial Keratotomy (RK)
» infectious keratitis unresponsive to medication
Advantages:
» Closed eye surgery
» No chance of potentially blinding endothelial rejection because the recipients own descemet’s membrane and endothelial cell layer is retained
» Can potentially repeat DALK or perform PK if the results of the original procedure are not satisfactory
» Better control of post-operative astigmatism particularly when large diameter grafts used.
Disadvantages:
» Conversion to full thickness PK may be required if perforation of descemet’s membrane – only 0.018 mm thick, about the thickness of cellophane, but not nearly as strong!
» Irregular astigmatism less common than PK but still possible
» Technically challenging
» Significantly longer operative time
» Offered by few cornea surgeons